Updated 29 April 2020
This page details the control strategies for the MIT Emergency Ventilator. Other control strategies with increasing complexity may be implemented at developer discretion and with clinical input.
Notice: Any control strategy must fulfill the requirements described in Key Ventilation Specifications.
The goal of the high-level controller is to provide a controlled volume of air to the patient in a set amount of time. There are two control phases: the inspiratory phase and the expiratory phase (see Figure 1). There are three input parameters, referencing the Key Ventilation Specifications:
Control Knobs
Tidal Volume (VT): The total volume of air to be delivered to the patient.
BPM: Breaths per minute, also called respiratory rate (RR). Typically varies between 8-30 BPM.
I/E Ratio (1:IE): The ratio of the duration of the inhale to the duration of the exhale. For example, a 1:3 ratio means that the exhale phase lasts three times longer than the inhale phase. Typically varies between 1:1 to 1:3, with a maximum of 1:4 currently being observed in COVID-19 patients.
Trigger Sensitivity: This setting is relevant to the assist control mode, and specifies the pressure threshold below PEEP for triggering a patient-triggered inhale cycle. See Clinical page.
In addition to these inputs set by the clinician, the high-level controller uses two more inputs: the motor encoder position and the system pressure. Its job is then to translate all these inputs into the motor commands the low-level controller needs: desired motor speed and position.
Note that because our device does not directly measure volume, the tidal volume (VT) input of our controller is specified as a percent of a full compression of the Ambu bag instead of Liters. The percent (%) of bag compression from 0 – 100% maps to the encoder pulses that correspond to how far the fingers of the device move towards or away from each other and this determines the volume of air delivered.
Calculating Waveform Timing & Durations
The pressure signal looks in particular as follows:
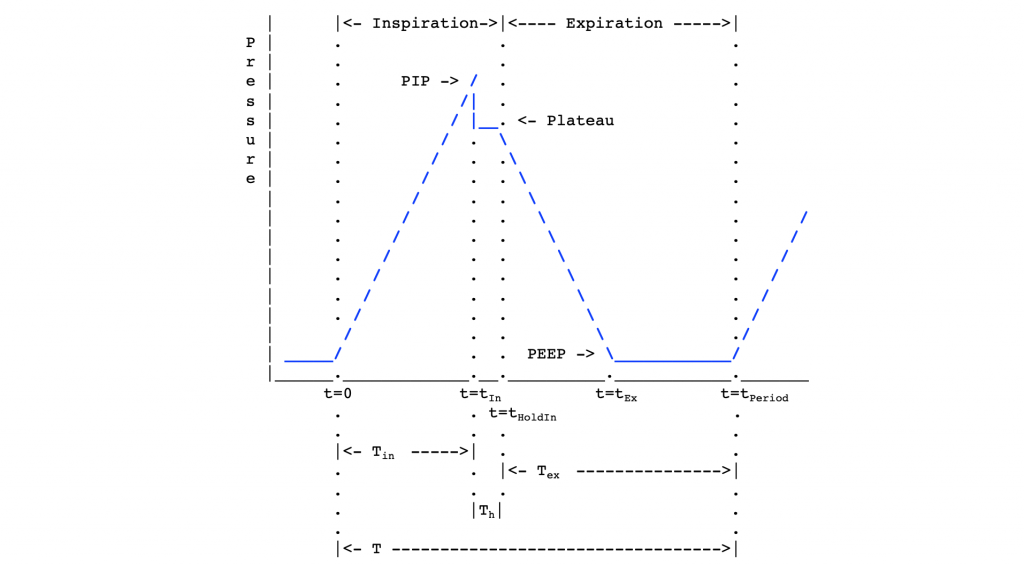
As a function of the three tunable inputs VT, BPM and IE, our controller determines the following timing durations noted in the waveform above:
Period (T): The duration (in seconds) of an inhale/exhale cycle.
T = 60 / BPM
Th: The duration (in seconds) of an inspiratory hold or pause at the end of inhale during the inspiratory phase for plateau pressure. This is usually a pre-determined constant that is not tunable.
Tin: The duration (in seconds) of the inhale time of the inspiratory phase.
Tin = T / (1 + IE) – Th
(Note: Here IE represents the ratio between Inspiration and Expiration, e.g. if I/E is 1:3 then IE is 3)
Tex: The duration (in seconds) of the expiratory phase.
Tex = T – (Tin + Th)
In addition to the timing parameters, the controller determines the following rotation rates:
Vin: The rotation rate of the inspiratory phase (in pulses/second).
Vin = VT / Tin
Ve: The rotation rate of the fingers in the expiratory phase (in pulses/second). Note that during exhalation, our device does not control flow rate out of the patient. This velocity is simply the velocity of the fingers opening and is not related to expiratory flow rate.
In addition to timing and rotation rates, there are four measurable pressure parameters that must be taken into account (see Figure 2):
Pmax: The maximum allowable pressure (set to 40 cmH20). A pop-off set for that threshold is usually provided for safety – see plumbing.
PIP: The Peak Inspiratory Pressure (PIP) is the maximum pressure during inhale. We consider 40 cmH20 to be the upper pressure limit for safety. This also corresponds to the over-pressure release valve limit on some Ambu bags.
Pplat: The plateau pressure of the inhale. An important diagnostic number for clinicians.
PEEP: The PEEP (positive end-expiratory pressure) is a residual pressure in the system after exhale. We do not directly control this value, but it is typically controlled manually via a PEEP valve on the Ambu Bag.
State Machine Summary
With time t being the amount of time spent in the current cycle. The waveform timings and pressure readings are then used to control a state machine that switches between phases in the control loop (see Figure 2).
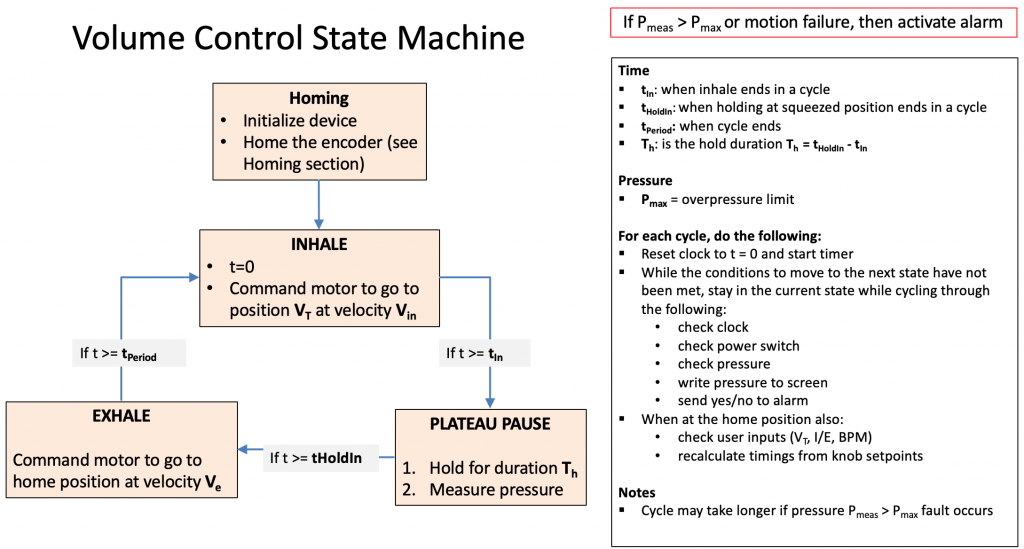
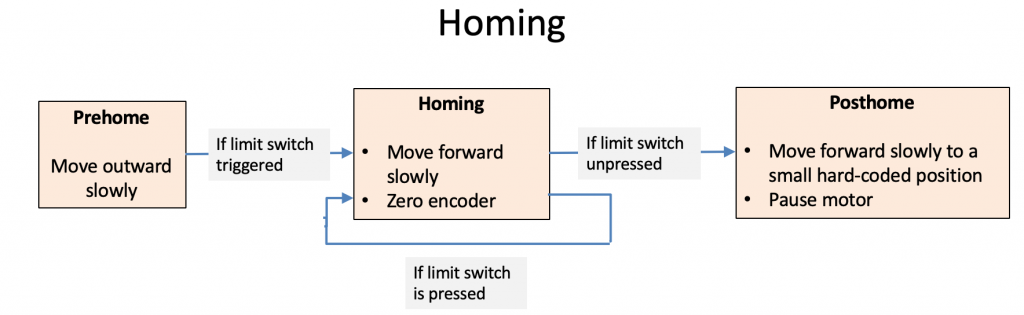
During the setup phase, we initialize the program, start serial communication with the motor controller, and home the encoder.
In the inspiratory phase, we command the motor to go to position VT at velocity Vin. After Tin seconds, we switch to the pause state.
In the pause state, we hold for time Th and measure the plateau pressure. We then switch to the expiratory phase.
In the expiratory phase, we command the motor to go to position 0 at velocity Ve. After time Tex, we switch back to the inspiratory phase.
Plateau Pressure
Each time the arms close, we implement a 0.10 s pause before they open. This does not affect the I/E ratio, but it is necessary to hold the air into the patient. During this phase the airway pressure is measured and displayed. This indicates “plateau pressure” and will guide clinical decision making. This pressure will be displayed until the next cycle and update.
Alarms Functions
See our List of Alarms.
All alarms must simply, concisely, and clearly alert the clinician of the type of fault, so that the clinician can decide how to proceed. For example, a mechanical fault requires a different clinical response than a patient who stops breathing on assist mode.
Alarms specifically related to pressure sensing are also describe in Pressure Measuring.
Assist Control
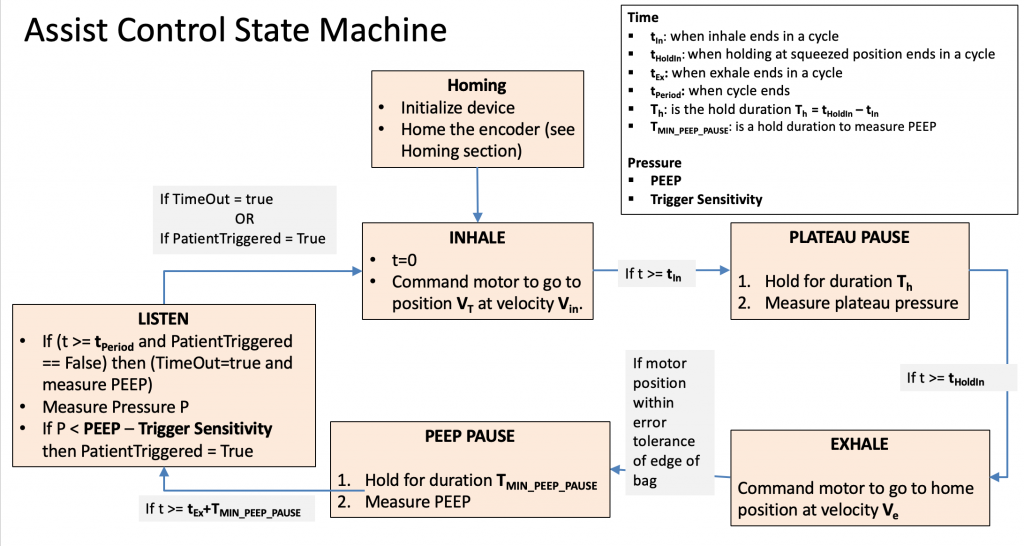
Assist Control differs from regular volume control in that the Exhale state is split into 3 states. In the first Exhale state, the fingers move to their home position at the edge of the bag. In the second state, Exhale Pause, the fingers pause for a short time and measure the PEEP. In the third state, Listen, we wait either for the patient’s own inhalation to trigger the Inhale state, or we wait for a set amount of time (like in normal Volume Control) and then trigger the Inhale state automatically. Read the Clinical page for more information.
In the Assist Control mode, a notification (not necessarily a full alarm) should also sound whenever a breath is NOT activated by the patient and the system’s timer kicks in to command a breath. Other faults must be detected, such as mechanical failures to reach desired positions, etc.

Recent Comments